Cancer Cells Wield ‘Nanotubes’ to Destroy the Immune System

Scientists discover microscopic nanotubes which allow cancer cells to attack the body’s immune system.
Cancer grows stronger by evading the immune system. A new study sheds light on how cancer cells can debilitate the immune system and metastasise.
New research published by Nature Nanotechnology suggests that cancer cells have a supervillain-esque strategy. The cancer cells attack by extending tiny tentacles into the immune cells to capture the mitochondria.
The mitochondria are the immune cell’s source of power, their lifeline. Without it, they are unable to continue protecting the body.
The stolen mitochondria boost the cancer cells and leave the immune cells wholly depleted.
“Cancer kills when the immune system is suppressed and cancer cells are able to metastasise, and it appears that nanotubes can help them do both,”
Said the study’s co-author Shiladitya Sengupta, PhD, and co-director of Brigham’s Center for Engineered Therapeutics, USA.
“This is a completely new mechanism by which cancer cells evade the immune system and it gives us a new target to go after.”
Nanotubes visible at a microscopic level
Sengupta and colleagues investigated cancer cells at the nanoscale level by setting up an experiment to co-culture breast cancer cells and immune cells, such as T cells. Utilising a state of the art microscopy technology, they noticed something extraordinary.
Cancer cells and immune cells were physically connected by tiny tendrils. One tendril is about the width of 100-1000 nanometres. To put this into perspective, one human hair is around 80,000 to 100,000 nanometres.
The researchers developed a process to test a cancer cell’s ability to destroy an immune cell. First, the team stained the mitochondria with a neon green dye. Then, they watched as the bright green mitochondria were sucked out of the immune cells, through the nanotubes, and into the cancer cells.
“It was very exciting because this kind of behaviour had never been observed before in cancer cells. This was a tough project as the nanotubes are fragile and we had to handle the cells very gently to not break them.”
Said Hae Lin Jang, PhD, co-author and a principal investigator in the Center for Engineered Therapeutics.
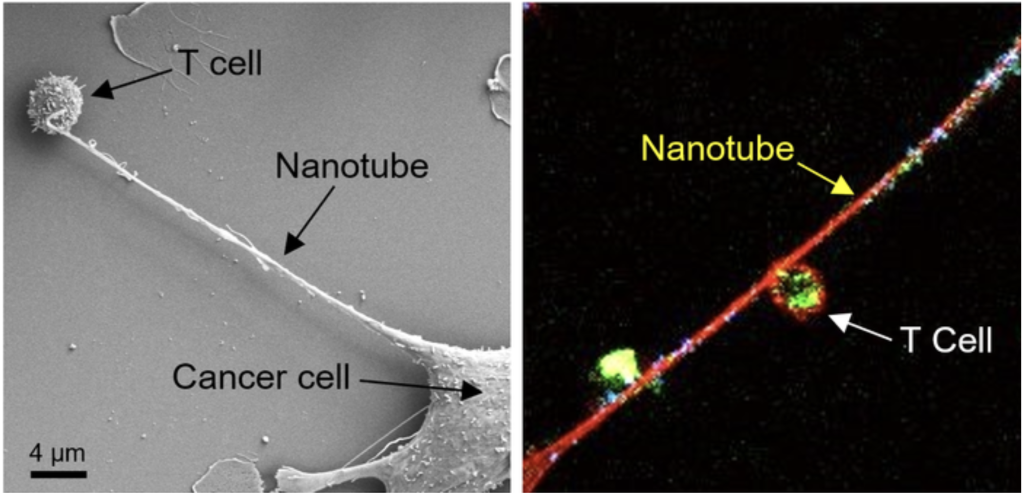
Left: Field emission scanning electron microscopy (FESEM) image shows the formation of a nanotube between a breast cancer cell and an immune cell. Right: Confocal microscopy image shows mitochondria (labelled with green fluorescence dye) traveling from a T cell to a cancer cell through the intercellular nanotube. DNA in the mitochondria was labelled with blue dye.
Credit: Nature Nanotechnology https://doi.org/10.1038/s41565-021-01000-4
Turning research into treatment
After this discovery, the researchers tested whether preventing the cancer cells from capturing the mitochondria would have any effect.
When they injected an inhibitor of nanotube formation, the cancer cells stopped growing and started shrinking.
“Based on our observations, there is evidence that an inhibitor of nanotube formation could be combined with cancer immunotherapies and tested to see if it can improve outcomes for patients.”
Said lead author Tanmoy Saha, PhD, a postdoctoral researcher in the Center for Engineered Therapeutics.
Knowing how cancer cells behave dramatically impacts our ability to invent new early detection technologies and treatments.
To help enable earlier detection, we are working hard to make our PanTum Detect test available in the UK. We are currently discussing potential partnerships with labs and clinics around the UK.
PanTum Detect can detect all cancers via a simple blood test, making it affordable and accessible for a primary care setting.
If you would like to partner with RMDM or find out more about PanTum Detect, please get in touch via our contact form.
Resources:
https://www.eurekalert.org/news-releases/935174